
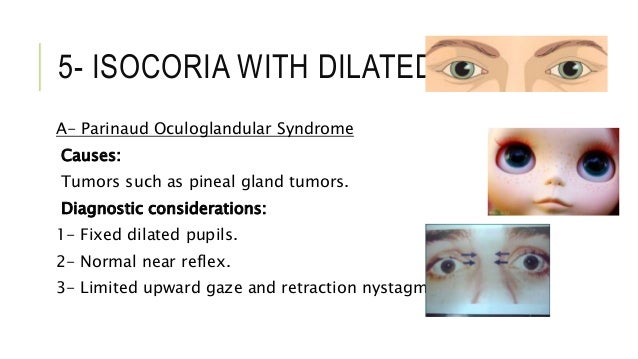
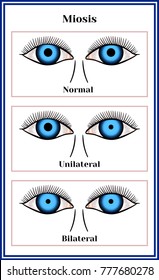
So, the emergency physician must be skilled in rapidly identifying those patients requiring further diagnostic procedures such as neuroradiological investigations, which could be superfluous and potentially dangerous in the developmental age. In fact, these disorders present with a wide variety of clinical pictures and underlie different etiologies, both congenital and acquired (head injury, infectious diseases, neurological and neoplastic diseases, toxic substances (systemically administered or topically instilled), vascular and autoimmune diseases), with different incidence rates compared to adults. The clinical manifestations of such disorders are represented by strabismus, ptosis, mydriasis (unilateral or bilateral) and miosis, with isolated or associated presentations. Although most of them involve non-LT conditions, the ED physician should consider potential “red flags” for appropriate management of children such as age > 6 years, combined OMDs, extra-ocular symptoms and co-morbidity.Īcute ocular motility disorders (OMDs) are a frequent reason for admission to an outpatient general hospital or to a pediatric Emergency Department (ED). OMDs are not an uncommon presentation at ED. LT etiologies were 16 times more likely in combined OMDs ( p = 0.018), were over 13 times more likely to report associated extra-ocular signs/symptoms ( p = 0.017) and over 50 times more likely to report co-morbidity ( p = 0.017). In a multivariable analysis, LT conditions included especially children over 6 years of age, increasing the odds ratio by 2% for each months of age ( p = 0.009). The majority of acute OMDs involved no underlying LT conditions ( n = 136) and most of them were infants or toddlers (50%). Of 192 visits for OMDs, the isolated strabismus occurred most frequently (55.6%), followed by pupil disorders (31.8%), ptosis (5.2%) and combined OMDs (11.5%). A subgroup analysis was performed comparing children with and without LT conditions. MethodsĪ retrospective cohort study evaluated children (2 months-17 years) admitted to a tertiary Emergency Department in 2009–2014. The aim of the study was to assess characteristics of children with acute Ocular Motility Disorders (OMDs), and to identify “red flags” for recognition of underlying life-threatening (LT) conditions. The emergency physician must be skilled in rapidly identifying patients with potentially life threatening (LT) forms, requiring further diagnostic procedures. Acute ocular motility disorders (OMDs) in children admitted to Emergency Department (ED) represents a not so rare condition with a wide spectrum of different etiologies.


 0 kommentar(er)
0 kommentar(er)
